Living With Arthritis Pain: What You Can Do
Chronic pain from arthritis often lasts for many months or for a lifetime. This degree of pain can strongly affect you on a daily basis. Chronic pain is more difficult to manage and treat when compared to acute pain. Chronic pain takes on a life of its own and is more than just pain symptoms.
When you have chronic pain, you can have limitations in activities of daily living (grooming, bathing, household chores, and cooking) and often have increased stress that can affect all areas of your life.
Pain, according to many people, is a symptom that has an underlying cause for being there. Once the underlying cause is treated, the pain should go away and you will feel better. For example, people with rheumatoid arthritis can be treated with biologic therapy or disease-modifying drugs (DMARDs), which can effectively decrease the pain in the joints. Another example is having a joint replacement surgery when you have osteoarthritis. The pain will often decrease but will not go away altogether.
While medical treatment can do a lot toward reducing the arthritic pain you are likely experiencing, there is often some type of residual pain. Why residual pain occurs under situations of chronic pain is not completely clear. Treatments to completely eliminate the pain are often difficult to come up with.
The Brain In Chronic Pain Syndromes
Research studies have indicated that chronic pain causes changes in the brain’s structures. Researchers now believe that chronic pain takes on a life of its own, becoming a disease that does not just involve the experience of pain. Even though the pain is located in the joint, the pain isn’t the only thing you will experience.
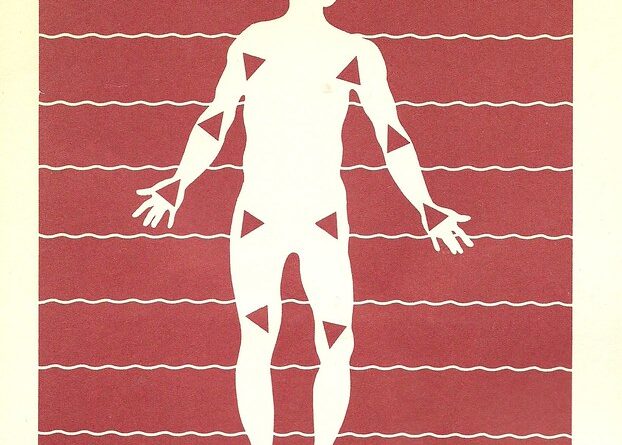
Chronic inflammation from rheumatoid arthritis, for example, causes pain signals to continuously bombard the brain. The nerve cells that carry the pain signal are secondarily changed so that they become more efficient at relaying the pain signals. The end result is that minor pain may be perceived by the brain as a significant pain. When this happens, it is called having “centralized pain.”
About 1/5 of all patients with osteoarthritis who underwent a replacement of their hip or knee report ongoing chronic pain. The pain becomes centralized and is not caused by the injury or the arthritic inflammation. This is also typical of the pain found in fibromyalgia. The pain starts in the connective tissue and ligaments but spreads to involve central nervous system, which is typical of centralized pain.
Coping With Arthritis Pain
Now that doctors have determined that arthritis pain and other chronic pain syndromes are much more than just inflammation and the perception of pain, they are using other modalities to treat the pain that extend beyond just treating the pain.
You can work with your doctor to find out which treatments can be helpful in dealing with the brain issues seen in chronic pain.
You can help control the pain and live better with arthritis if you practice the following:
• Try not to suffer.
Chronic pain is defined as pain that has been going on for at least three months or pain that lasts past the time the injury would be expected to heal. You need to take action toward reducing the pain before it turns into chronic pain. It is easier to treat short-term pain than it is to treat chronic pain. It means that you might want to take pain relievers early in the course of your illness so that the pain can be quickly relieved while it is acute so it doesn’t cause the brain changes seen in chronic pain.
• Talk to your doctor.
When talking to your doctor, you need to relay as much information about your pain as possible even if your doctor doesn’t seem to be getting it. Tell the doctor where you are experiencing the pain, what the pain feels like, and how long you have had the pain. Tell the doctor about what limitations you are experiencing because of the pain. Try keeping a diary in which you explain those situations that worsen or improve the pain. Let the doctor read the diary so he understands the impact of pain on your life.
• See a pain center.
If your doctor is not giving you adequate relief of pain, you may need to seek the advice of specialists at a pain clinic. A good pain clinic has a multidisciplinary team on its staff, including a psychiatrist, an anaesthesiologist, psychologists, physical and occupational therapists, and physiatrists.
• Try central nervous system medications.
There are alternative medications you can take for chronic pain that act on the brain. These include Cymbalta and Lyrica, which are used to treat other medical conditions but are also helpful in chronic pain conditions. These drugs act on neurotransmitters, like serotonin and norepinephrine, which play a role in well-being as well as on the perception of pain.