What is Rheumatoid Arthritis ?
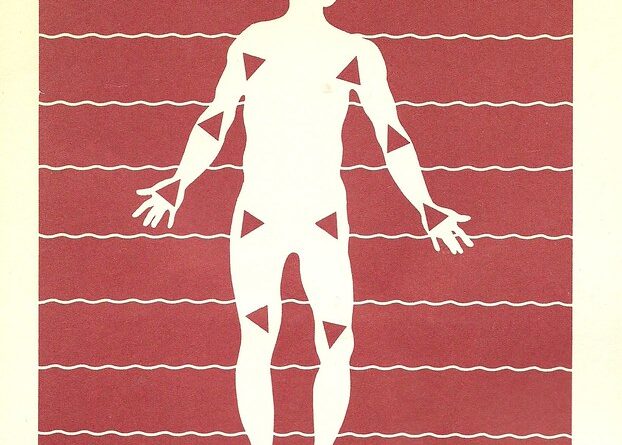
Rheumatoid arthritis is an autoimmune disease that results in chronic inflammation and pain in the smaller joints, such as those in your feet and hands. It differs from the more common osteoarthritis in that rheumatoid arthritis doesn’t come from wear and tear on the joints but instead affects the synovial lining of the joints so that they swell and become inflamed. Eventually, the cartilage wears away and you end up with bony erosion of the joints and severe joint deformity.
As an autoimmune disorder, rheumatoid arthritis happens when the immune system attacks the tissues of the body, in this case, the tissues within your joints. Some people with rheumatoid arthritis develop symptoms in other body areas, when the autoantibodies affect the eyes, blood vessels, skin, and lungs.
Rheumatoid arthritis has been known to affect children but it is usually a disease-affecting people older than 40 years of age. Like all autoimmune disorders, the disease is more common in women than it is in men. Treatment, as you will see later, is focused on reducing your symptoms and preventing further damage to your joints.
Signs And Symptoms Of Rheumatoid Arthritis
If you have rheumatoid arthritis, these are some things you can expect:
• Joint stiffness that is usually worse in the morning but can last for several hours throughout the day
• Joints that are tender to the touch, warm, sometimes reddened, and swollen. As mentioned, this usually involves the smaller joints of the body.
• Lumps of tissue beneath the skin near the joints. These are called rheumatoid nodules and may or may not be painful to the touch.
• Weight loss, fever, and fatigue. These are the natural effects of autoantibodies in the body tissues.
• Swollen PIP joints. These joints connect the hands to the fingers. Eventually the joints of the feet are affected as well. Wrists, ankles, elbows, shoulders, and hips will eventually become affected by this disease. The disease is usually bilateral, meaning that they affect both sides of the body at the same time.
You may have steady symptoms of rheumatoid arthritis or may have symptoms that come and go. Rheumatoid arthritis is characterized by flares of increased joint inflammation with periods of time where the joints are less affected. The longer you have rheumatoid arthritis, the more likely it is that you will have joint deformities that do not go away.
Causes Of Rheumatoid Arthritis
Rheumatoid arthritis is an autoimmune disease, which means that your body has made antibodies in the immune system that attack the tissues that line the joints. The synovium or joint lining becomes inflamed and thickened. Eventually the cartilage becomes destroyed, leaving bone to rub on bone. In the most severe cases, the bone itself will erode as well.
The ligaments and tendons that connect the joints to other tissues will stretch out and weaken so that the joint itself begins to become deformed. Exactly how this autoimmune process works is not clear. There may be both environmental and genetic factors playing into who gets rheumatoid arthritis and who doesn’t. It’s possible that genetics interacts with environmental things like infections to result in the disease.
Risk Factors For Rheumatoid Arthritis
There are certain factors in your life that may make it more likely that you’ll get the disease. These include the following:
• Family history.
If a parent or sibling has rheumatoid arthritis, this may put you at an increased risk of getting the disease.
• Gender.
If you are female, you have a greater chance of getting the disease.
• Age.
While it can occur in a person of any age, most people are diagnosed with rheumatoid arthritis between 40 and 60 years of age.
Complications Of Rheumatoid Arthritis
Rheumatoid arthritis isn’t just a disease of the joints. There are several complications of the disease that you should be aware of. These include the following:
• Lung disease.
If you have rheumatoid arthritis, you stand a greater chance of also having scarring and inflammation of your lungs, which can cause you to feel short of breath.
• Osteoporosis.
You can get thinning of your bones just because you have rheumatoid arthritis. Alternatively, some of the medications used to treat the disease can cause weakened bones.
• Heart problems.
People with rheumatoid arthritis have a greater chance of having blocked arteries in the heart and an increased chance of pericardial sac inflammation.
• Carpal tunnel syndrome.
If you have rheumatoid arthritis in the wrist area, it can compress the carpal tunnel, which houses the median nerve. This can result in tingling and numbness of your hands and fingers.
Tests For Rheumatoid Arthritis
In the early stages of the disease, rheumatoid arthritis can mimic other joint diseases, making it difficult to diagnose the disease. A careful physical examination by your doctor, however, might show characteristic findings of rheumatoid arthritis, including swelling of specific joints in the hands and the presence of rheumatoid nodules.
There is a blood test for rheumatoid arthritis that can clinch the diagnosis. It is called the “rheumatoid factor,” which is a test that detects the autoantibodies that are acting on your joints. Other tests for inflammation can help aid in the diagnosis of the disease.
There are characteristic x-ray findings for rheumatoid arthritis. The joints will look deformed and there will be a lack of joint space noted on x-ray as the disease progresses.
Treatments For Rheumatoid Arthritis
Because there is no cure for rheumatoid arthritis, the treatment is directed at controlling your symptoms and helping you feel better. There are some medications that will slow the degree of joint damage you will experience.
There are several types of drugs used in the treatment of rheumatoid arthritis. Some are relatively easy to tolerate, while others have serious side effects that you should be aware of. Doctors usually start with the medications that are easiest to tolerate first. Here are some good treatments for rheumatoid arthritis.
• Steroids.
Steroid medications, such as prednisone or prednisolone, are helpful in that they reduce the pain and inflammation of the joints and can reduce the rate of joint damage. Unfortunately, they have side effects, such as osteoporosis, diabetes, and weight gain. Steroids are especially good when you have flares of the disease and are not meant to take chronically.
• NSAID medication.
These include medications like ibuprofen and naproxen (unless you get one prescribed by the doctor). They are not without side effects, however, and these include liver damage, kidney damage, irritation of the stomach, heart problems, and tinnitus.
• Anti-Rheumatic drugs.
These medications can actually lessen the damage done by the autoantibodies so that the joints aren’t permanently damaged. Medications in this class include Plaquenil, Azulfidine, methotrexate, and leflunomide. Because they can affect your immune system, they can cause side effect including suppression of your bone marrow, lung infections, and liver problems.
• Biologic medications.
These represent a new class of medications that act on the immune system so that there is less inflammation and less joint damage. They can cause an increase in infections because they affect the immune system. Choices of biologic medications include adalimumab, abatacept, certolizumab, rituximab, and infliximab.
• Physical therapy.
You may wish to see a physical therapist who can help you learn various exercises that will keep your joints more flexible. They may also help you learn how to do things around the house that don’t involve using your hands. Assistive devices may be prescribed for you that will help you do things without stressing the joints too much.
• Surgery.
Surgery can be done that can repair the damage to your joints. This includes things like joint replacement in which the damaged joints are removed and a prosthetic joint is put in its place. Tendons can also be repaired. In the worst case scenario, the surgeon can fuse the joints together so they don’t rub against one another.


